Tejpaul S. Pannu, M.D.
Neurosurgeon
The cervical vertebrae are the part of the spine we use the most on a daily basis to go about our normal lives, and are made up of the top seven bones in your spinal column. Understanding these vertebrae, including what can go wrong with them and how problems can potentially be avoided, can help you decide if your cervical vertebrae may benefit from specialized care due to chronic pain or injury.
The Function of Cervical Vertebrae
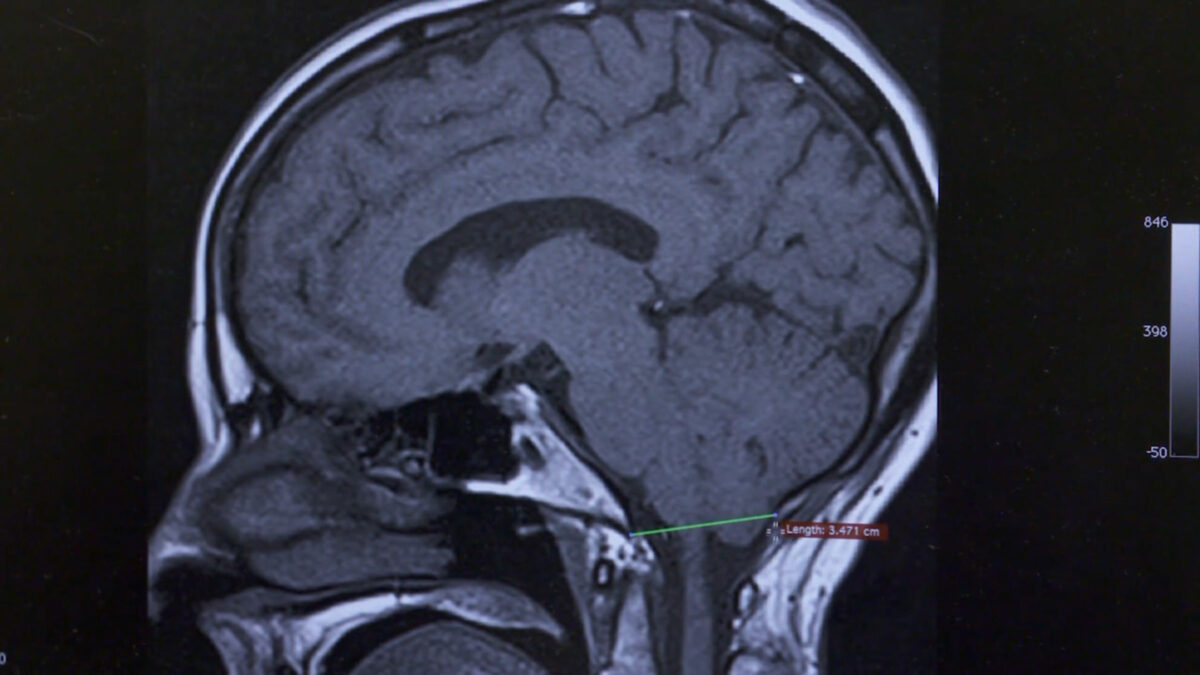
In addition to protecting the spinal cord, which contains nerves that send signals throughout the body from the brain, the cervical vertebrae play a key role in flexibility and mobility.
The two uppermost cervical vertebrae connect to the skull and are critical for turning our heads side to side and up and down. The cervical vertebrae also serve as a conduit for the nerves that go into your hands and arms, so when there’s pain or disfunction from your cervical vertebrae, there’s a good chance you’ll feel it in your extremities, too.
In general, these seven vertebrae flex and move more and differently than any other part of the spine. Just sitting and having a conversation with a friend, you’re going to use your cervical spine much more than the rest of your spinal column.
What Can Go Wrong with Cervical Vertebrae?
Problems with the cervical vertebrae can be congenital, meaning a person is born with them, or they may arise as a result of degeneration due to injury and/or the general wear and tear caused by aging.
Sometimes people don’t know they have a congenital spinal issue until later in life, when they start having pain or other symptoms. As you get older and your skeleton starts to age, issues come to the forefront that may have never bothered you before. Other congenital conditions that affect cervical vertebrae, such as congenital cervical spinal stenosis, may never cause any symptoms.
Due to gravity and upright walking and sitting, we all experience some degeneration of the cervical vertebrae. Injuries to the spine can also add up over the course of a person’s lifetime, exacerbating degeneration. And an accident or fall can cause sudden and acute damage to the cervical vertebrae.
Cervical issues tend to be more problematic than those affecting other parts of the spine because the cervical vertebrae are closest to your brain. All inflammation starts in the brain and works its way down through the spinal cord, so compression of the cervical vertebrae can cause problems as varied as hand numbness, bladder urgency and gait instability.
Managing Neck and Spine Issues
Whether the damage happens gradually or all at once, problems in the cervical vertebrae can be effectively addressed in several different ways.
The first thing a neurosurgeon will want to do is assess your symptoms, including levels of pain, weakness, and numbness as well as ability to perform tasks such as grasping and walking. Depending on the type and severity of your symptoms, your provider will work with you to decide on a course of treatment.
For mild to moderate symptoms affecting the cervical vertebrae, non-invasive treatments can work quite well. These include physical therapy, acupuncture, chiropractic adjustments, pain injections and laser therapy.
For more serious cases — if your pain is so bad that it affects your ability to function, or if you’re having trouble walking, with or without falling — a specialist may recommend surgical intervention. Surgery may also be considered if you’ve tried less invasive treatments without success. Cervical vertebral surgeries, many of which are minimally invasive, tend to have a very high success rate.
When to See a Specialist
You may not give your cervical vertebrae much thought until they start to trouble you, but this small set of bones does a big job.
Because the cervical vertebrae are so critical for spinal and overall health, it’s a good idea to check with your general practitioner if you have neck pain that lasts for more than a couple weeks, or if you’re experiencing any type of weakness, numbness (also called neuropathy) or difficult grasping or holding objects.
You can also go directly to a specialist who can perform a thorough evaluation and design a treatment plan for your specific needs.
If you or a loved one is seeking treatment for neck and spine issues, or to schedule an appointment with Dr. Pannu or any of our MHSI experts, visit www.mhsi.com/appointments or call 248-784-3667.