Neuromodulation: A New Tool for Pain Relief
Approximately 50 million people in the United States — one in five adults — report struggling with pain on most days or every day. This type of chronic pain can interfere with every aspect of life, making even the simplest of tasks unmanageable.
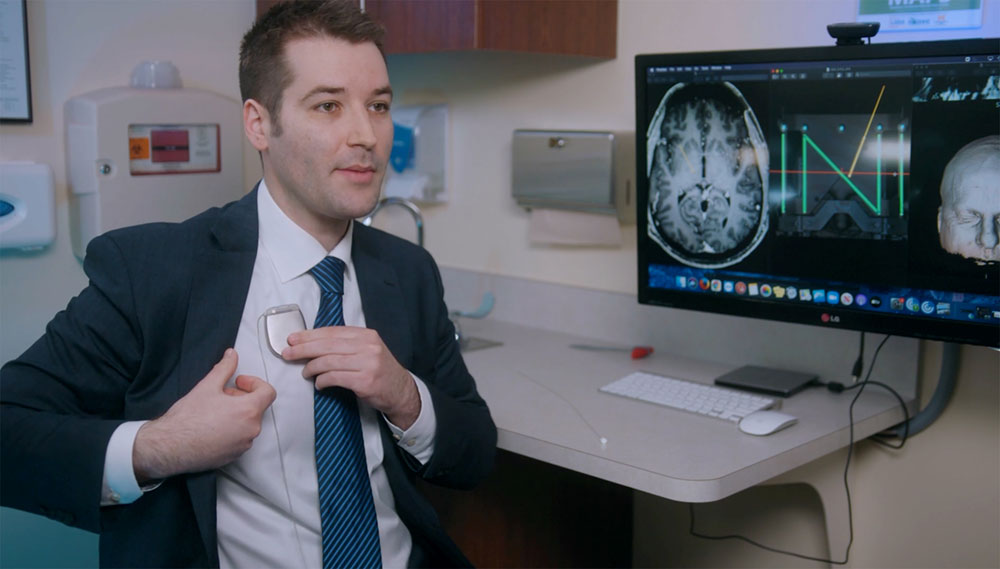
Fortunately, recent advances in technology have resulted in a new tool for treating chronic pain called neuromodulation. Understanding this treatment, including what it involves and how it works, may help you decide if neuromodulation is right for you.
What is Neuromodulation?
Neuromodulation refers to altering or modulating the function of the nervous system using targeted electrical stimulation or drug delivery. This can be accomplished using non-invasive devices such as transcutaneous electrical nerve stimulation (TENS) units or implantable devices such as spinal cord and deep brain stimulators.
The nervous system can be targeted anywhere along its course, including the brain, spinal cord or peripheral nerves.
How Does Neuromodulation Help With Chronic Pain?
In simple terms, Neuromodulation alters or blocks pain signals as they travel to the brain. Depending on a patient’s pain pattern, the device can be placed at different locations in the spine or on certain nerves to block pain.
Chronic pain can be described as aching, sharp, stabbing or burning sensations. Neuromodulation devices override these sensations, instead providing a soothing or gentle tingling feeling in painful areas.
Can My Pain Be Treated With Neuromodulation?
Ideal candidates for neuromodulation for pain are those with chronic (not acute) pain, usually defined as pain lasting more than 3 months. This is typically pain that affects the neck, back or extremities, although there are options for facial pain and other pain patterns as well.
These patients have usually tried different medications or injections and continue to experience pain. Many have had back or neck surgery and continue to have pain, and others don’t qualify for surgery or don’t want to have additional or more invasive surgery.
What Happens During the Procedure?
For spinal cord stimulation, patients require a “trial” before the permanent device is implanted to ensure that the therapy is effective and worthwhile. A trial of spinal cord stimulation typically involves placing thin electrodes through two needles into the back, similar to an epidural injection. These are threaded to the appropriate region that matches the patient’s pain pattern.
These electrodes are then connected to an external device and patient’s “trial” the therapy at home for about a week. If the trial is successful, meaning pain severity is reduced by at least 50%, the temporary electrodes are removed in office and the permanent implant is planned.
This next step involves placement of the same electrodes in the same location, although now they are anchored into the back and connected to a small battery which is also implanted into the back or buttocks through two small incisions in the back. For some patients, a small laminotomy (opening in the spinal vertebra) is necessary to place the electrode.
Deciding which devices are used and where they are implanted requires an individualized approach based on each patient’s unique needs and anatomy.
What Does Recovery Look Like?
These are almost universally outpatient surgeries, and patients tend to experience some slight post-operative discomfort which resolves after a few days.
Patients should limit twisting, bending and lifting more than 5-10 pounds for the first two weeks after implantation to allow for healing, and for the electrodes to scar or “set” into place.
Once patients are seen at their first post-operative visit, we typically discuss a gradual return to activity and lifting of restrictions. Patients also have their devices programmed at that time, during which we map their pain distributions with the stimulation.
Are There Risks Associated With Neuromodulation?
Infection is the most common complication, particularly with implantable devices; on average this risk is 2% for any infection. Important risk factors that can contribute to infection are diabetes, smoking and obesity.
The risk of a spinal fluid or cerebrospinal fluid (CSF) leak is approximately 1%. The risk of a devastating complication such as spinal cord injury is very rare, occurring in much less than 1% of cases.
Although almost all neuromodulation devices currently manufactured and implanted are MRI-compatible, certain precautions must be taken in terms of what type of MRI machine can be used.
Who Else Can Benefit From Neuromodulation?
In addition to chronic pain, neuromodulation devices are often used for movement disorders such as tremors, Parkinson’s disease and dystonia. Additional conditions that can be treated with neuromodulation include obstructive sleep apnea and urinary incontinence.
Neuromodulation also has a long history of use for psychiatric disorders, including obsessive compulsive disorder and depression.
Pain Relief is Possible
Patients with complex regional pain syndrome tend to do very well with spinal cord stimulation, and my last patient was a young woman who went from being unable to walk on her own feet to regaining full strength and having greater than 90% pain relief.
For deep brain stimulation, it’s very gratifying to test the stimulator in the operating room with the patient awake—one of my more recent patients started crying when she realized that her tremor was completely gone for the first time in decades.
If you or a loved one are dealing with chronic pain and feel like you’ve tried everything, talk to a healthcare provider about neuromodulation. You may be only one outpatient procedure away from finally finding relief.